Root Canal Treatment (Endodontics)
Root canal treatment relieves pain and saves teeth.

When a dentist or endodontist tells the need for root canal treatment, the term “root canal” itself may send shivers down spines due to preconceived notions that root canal treatment is filled with pain and discomfort which are nothing more than outdated myths . In fact, root canal treatment doesn't cause pain but actually relieves it. Advances have made the treatment a virtually pain-free experience, many times accomplished in a single visit. so, don’t worry… you're not alone. Millions of teeth are treated and saved each year with root canal, or endodontic treatment. So let's start by dispelling a common myth: Root canal treatment doesn't cause pain — it relieves it!
One can gain more information by going through this step-by-step walk-through of root canal treatment.
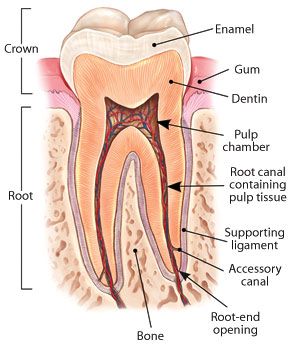
This is how a normal, healthy tooth anatomy is-
This is how a normal, healthy
Inside the tooth, under the white enamel |
|

|
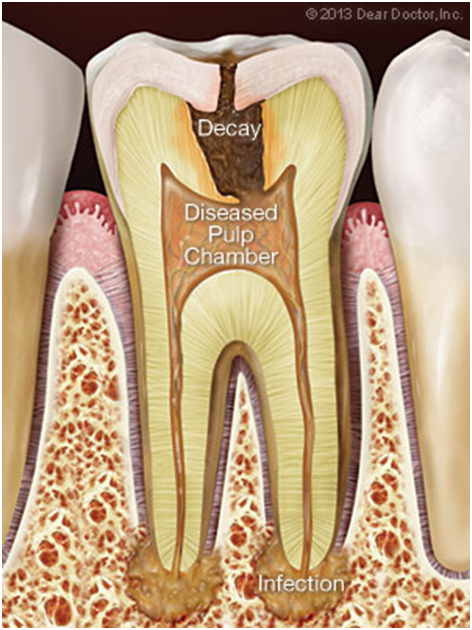
When is root canal treatment necessary-
Root canal or endodontic treatment (endo-inside, dont-tooth) is necessary when the inside, or pulp of a tooth becomes inflamed or infected. The inflammation or infection can have a variety of causes: deep decay, repeated dental procedures on the tooth, faulty crowns, or a crack or chip in the tooth. In addition, trauma to a tooth may cause pulp damage even if the tooth has no visible chips or cracks. If pulp inflammation or infection is left untreated, it can cause swelling and pressure inside the tooth (that has nowhere to go), leading to tooth pain and swelling, eventually, irreversible damage to the pulp. Once the pulp dies, the pain may subside initially, sometimes to return as an acute (painful) infection spreading into the periapical tissues (“peri” – around; “apex” – end), particularly the bone. It could also become a chronic (long-standing) infection with symptoms ranging from mild to severe.
|
Generally speaking, whatever the cause of root canal or pulpal disease, root canal or endodontic treatment will be necessary to Endodontists are dentists who have completed an additional three years of advanced post graduate training in the diagnosis and management of diseases and disorders of the dental pulp, and in the diagnosis of dental pain; their focus is therefore on saving teeth. |
|

|
Q: What is the advantage of saving the tooth by going for root canal treatment?
Possible problem: The pulp tissue inside a tooth is acutely infected, inflamed and dying. This is generally in response to decay coming very close to or entering the nerve.
Saving the natural tooth with root canal treatment has many advantages:
 Efficient chewing
Efficient chewing
 Normal biting force and sensation
Normal biting force and sensation
 Natural appearance
Natural appearance
 Protects other teeth from excessive wear or strain
Protects other teeth from excessive wear or strain
 Maintains the integrity of arch n teeth, means position of other teeth is maintained. If the tooth is removed, neighbouring and opposing teeth can drift or shift the position, which can lead to cavities or mobility of other teeth. If the tooth is removed, replacement with artificial tooth is mandatory either with removable denture, bridge or implant
Maintains the integrity of arch n teeth, means position of other teeth is maintained. If the tooth is removed, neighbouring and opposing teeth can drift or shift the position, which can lead to cavities or mobility of other teeth. If the tooth is removed, replacement with artificial tooth is mandatory either with removable denture, bridge or implant
Hence Endodontic treatment helps you maintain your natural smile with natural teeth, continue eating the foods you love and limits the need for ongoing dental work. With proper care, most teeth that have had root canal treatment can last as long as other natural teeth and often for a lifetime or atleast for many decades.
Q: What are typical symptoms of root canal infection?
 Sharp, acute and intense pain, which is difficult to pinpoint
Sharp, acute and intense pain, which is difficult to pinpoint
 Sharp pain when biting down on your tooth or on food
Sharp pain when biting down on your tooth or on food
 Lingering pain after eating hot or cold foods
Lingering pain after eating hot or cold foods
 Dull ache and pressure
Dull ache and pressure
 Pain in lying down position or in the night time.
Pain in lying down position or in the night time.
 Tenderness (accompanied by swelling) in the nearby gums or on the face.
Tenderness (accompanied by swelling) in the nearby gums or on the face.
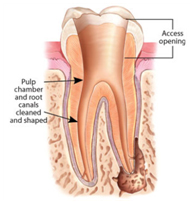
Q: How does the endodontic treatment procedure carried out?
A small opening in the chewing surface of your tooth is created to gain access to the pulp. Very small instruments are used to remove dead and dying tissue and clean the pulp from the inside, allowing the root canals to be cleaned and disinfected. The canals are specially “shaped” and prepared so that they can be sealed with biocompatible filling materials. They are coated with an adhesive cement to ensure that they are completely sealed to prevent future infection. After restoration, the tooth continues to function like any other tooth.
Contrary to jokes about the matter, modern root canal treatment is very similar to having a routine filling and usually can be completed in one or two appointments, depending on the condition of your tooth and your personal circumstances. You can expect a comfortable experience during and after your appointment.
It is becoming increasingly common today for root canal specialists to use microscopes for these intricate and detailed procedures to make the cleaning and shaping process more precise and efficient.


Q: What are the latest techniques and equipments used by dentists and endodontists to increase the outcome of treatment?
Endodontists and dentists today use state-of-the-art technology including digital (radiographic) imaging to diagnose root canal problems, and after treatment to verify that the canals are properly sealed; apex locator for accurate detection of the root end , endomotor and rotary files for efficient cleaning and shaping of infected teeth and roots, ultrasonic instrumentation to remove old canal fillings and posts and clean debries from root canals; lasers to sterilize the root canals, materials with properties of dissolving all necrotic tissues and medicaments to dry up all the infection in roots and surrounding bone and materials for airtight filling to prevent reinfection in the tooth are available today due to which the success rate of root canal treatment has gone very high in comparison with olden days. Most of the endodontists use operating microscopes ,which enlarges the working field to accurately locate, visualize and seal root canal systems ; it really is quite high-tech.
Q: how long will the root canal treated tooth last?
Today, root canal treatment, also known as endodontic treatment will save your natural tooth and allow you to keep it functional for decades if not a lifetime. With the development of latest techniques, But just as no two people are the same, teeth also vary widely, so that the success of root canal treatment depends on many factors.
Some Factors Affecting Root Canal Longevity
 How well the treatment has been done, meaning quality of treatment.
How well the treatment has been done, meaning quality of treatment.
 Teeth having first time root canal treatment contributed to the success and longevity of root canal fillings.
Teeth having first time root canal treatment contributed to the success and longevity of root canal fillings.
 Prognosis hampers in case of Teeth with more of infection spreading into the bone. in other words, the earlier the tooth is treated the better the outcome. So don’t put off treatment if you need it!
Prognosis hampers in case of Teeth with more of infection spreading into the bone. in other words, the earlier the tooth is treated the better the outcome. So don’t put off treatment if you need it!
How quickly and effectively the damaged tooth was repaired after root canal treatment was completed was also a factor, meaning it’s important to have the tooth restored with a permanent filling or crown, which usually requires a second office visit, without delay.
Q: If pulp keeps the tooth alive, How a pulpless tooth can survive and function?
The tooth is attached to the bone around it by the periodontal membrane or ligament (“peri” – around; “odont” – tooth), which is living, so that the tooth can still function even though the root canal system no longer contains its original tissue.
Q: Is it mandatory that every root canal treated tooth should be receiving crown?
Over time, teeth can become more brittle and have a greater tendency to fracture, especially the back molar teeth that receive the most biting force. That’s why it’s important to place crowns on root canal treated teeth to cover and protect them from undue stress, which will increase their longevity. Sometimes it is also necessary to place a post inside a treated root canal to support and reinforce a crown, especially if the tooth has been extensively damaged.
Q: What can I expect following the procedure?
In some instances for the first few days after treatment, your tooth may feel tender or sensitive, especially if there was pain or infection before the procedure. Most discomfort can be relieved by simple pain killers. avoid chewing or biting hard substances on the treated tooth until a crown or other permanent restoration is given further to protect and restore the tooth to full function and is extremely important in ensuring long-term success.
Q. Can an infected tooth cause a general body infection?
Root canal infection can spread into the bone immediately around the root end if left untreated, although it usually remains localized to the area. An association has been shown between periodontal (gum) and to a lesser extent, endodontic (root canal) infection and some systemic (general) body diseases, but it is rare in an otherwise healthy person.
Q: Who is qualified to perform root canal treatment?
All general dentists have received training in endodontic treatment and can perform most endodontic procedures, depending on their comfort level. Often they refer people needing complicated root canal treatment to endodontists, who have had specialized training of 3 years after the BDS .
Q. What is the advantage of opting for root canal treatment instead of bridge or implant?
Preserving Nature’s Gifts- Studies have shown that getting root canal treatment provides a longer-lasting solution than having replaced with fixed bridgework, for which the healthy neighbouring teeth need to be cut by 1.5mm- 2mm, which even can fail over time. The evidence for keeping a root canal treated tooth versus getting a dental implant is more equivocal, but that is a more complex issue involving other considerations besides longevity; it also includes more treatment time and costs. Certainly a tooth or teeth with well-treated root canal fillings and restorations will last for many years, if not a lifetime. Suffice it to say, there is nothing like your natural teeth.
Q. What is Root Canal Retreatment? When is it required?
Root canal treatment of a previously root canal treated tooth is called re root canal treatment.
As occasionally happens with any dental or medical procedure, a tooth may not heal as anticipated after initial treatment for a variety of reasons:
 Narrow or curved root canals sometimes pose complications during the initial procedure
Narrow or curved root canals sometimes pose complications during the initial procedure
 Complicated root canal anatomy (shapes and forms) went undetected in the first procedure.
Complicated root canal anatomy (shapes and forms) went undetected in the first procedure.
 The placement of the crown or other restoration was delayed following the treatment, resulting in reinfection of the root canals.
The placement of the crown or other restoration was delayed following the treatment, resulting in reinfection of the root canals.
 An inadequate seal of a restoration (filling) allowed recontamination of the inside of the tooth.
An inadequate seal of a restoration (filling) allowed recontamination of the inside of the tooth.
 New decay can expose the root canal filling material to bacteria, causing a new infection in the tooth.
New decay can expose the root canal filling material to bacteria, causing a new infection in the tooth.
 A loose, cracked or broken crown or filling can expose the tooth to new infection.
A loose, cracked or broken crown or filling can expose the tooth to new infection.
 A tooth sustains a fracture of the crown or root.
A tooth sustains a fracture of the crown or root.
Certainly a tooth or teeth with well-treated root canal fillings and restorations will last for many years, if not a lifetime. Suffice it to say, there is nothing like your natural teeth.
What exactly is done in retreatment?
First, all options should be reviewed, together with the risks, benefits and alternatives. Assuming the tooth can be retreated, it will need to be “reopened”. A small hole will be made into the biting or chewing surface of the tooth to gain access to the root canal. In many cases, complex restorative materials — crown, post and core material — must be “disassembled” and removed to permit access to the root canals. The previous root canal filling materials are removed and the canals cleaned and carefully examined, usually requiring magnification and illumination, which includes searching for any additional canals or unusual canals that require treatment. After cleaning and shaping the canals they will be sealed and a temporary filling or crown placed. If the canals are unusually narrow or blocked, there is a possibility that endodontic surgery may be necessary to treat infection and reseal the canal(s). Upon successful completion and healing of infection, a new crown or restoration will need to be placed on the tooth to protect and restore it to its full form and function.

How do I know if retreatment is the best choice and what are the alternatives?
Whenever possible, it is best to save your natural tooth. Retreated teeth can function well for years. Advances in technology are constant and updated techniques may be used to save a tooth, which may not have been available when you had your first procedure. If non-surgical retreatment is not an option, then endodontic surgery may be considered. This involves making an incision to allow access to the end of the root(s). Endodontic surgery may also be recommended in conjunction with retreatment or as an alternative. The only other alternative to retreatment or failing endodontics ultimately is extraction of the tooth. It will then need to be replaced with an implant, bridge or removable partial denture to restore chewing function and aesthetics and importantly, to prevent adjacent teeth from shifting. Because these options require surgery or dental procedures on adjacent healthy teeth, they can be more costly and time consuming than retreatment and restoration of the natural tooth.
Who performs root canal retreatment and what are the costs?
Endodontic or root canal retreatment can be more complicated and technically challenging than initial treatment, and can be carried out by any dental surgeon or by root canal specialists, “endodontists”. Most modern endodontic procedures are performed with the use of microscopes to allow the proper degree of precision and sophistication needed to ensure success. The cost varies depending on how complicated the procedure will be and the time that is needed. Teeth with multiple canals, like the back (premolar and molar) teeth will take more time especially if there are extra or unusually shaped canals. Restorations and filling material may also need to be removed to reaccess the root canal. The bottom line is that you should review all the risks, benefits and alternatives of root canal retreatment with your dentist or endodontist. You've already made an investment in saving your tooth. The payoff for choosing retreatment should be a healthy, functioning natural tooth for many years to come.
What is Apicoectomy procedure?
When a tooth cannot be successfully treated with conventional root canal treatment An apicoectomy is adviced along with root canal treatment, which is a minor surgical procedure in which the very tip of the tooth’s root is removed (“apico” – apex or end; “ectomy” – removal) and sealed.